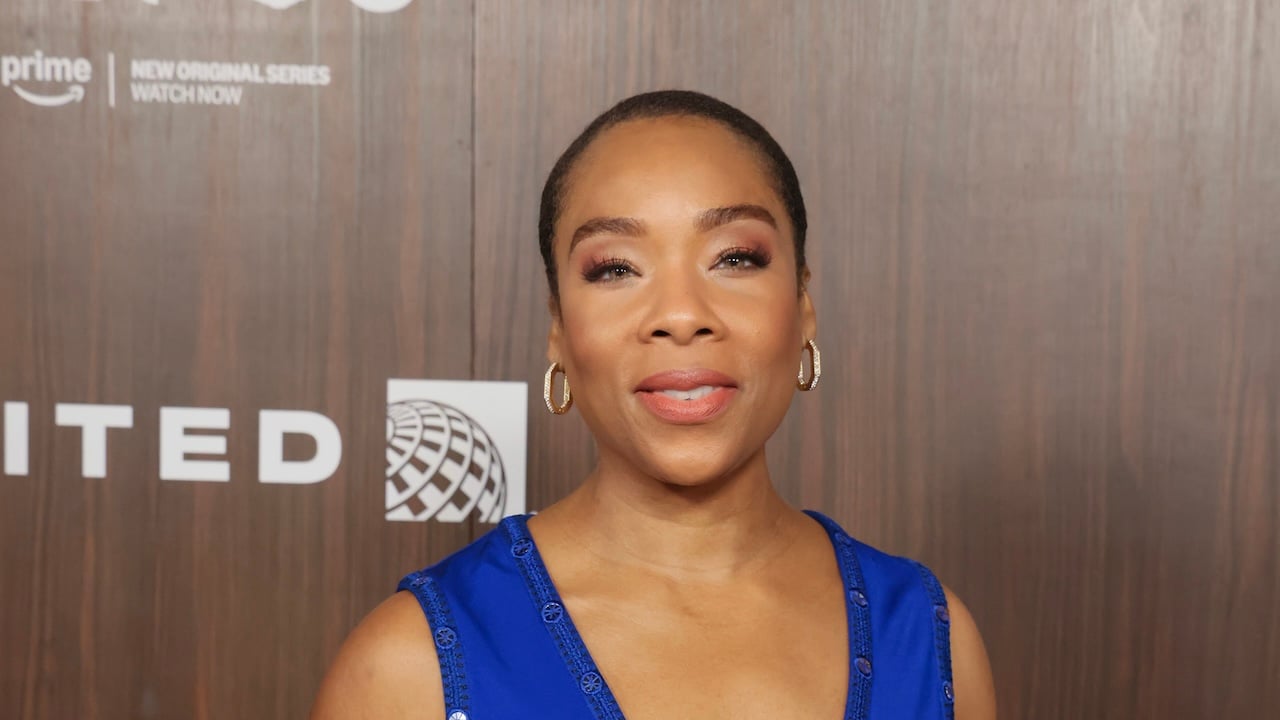
National Menopause Show Helps Women Navigate ‘The Change’
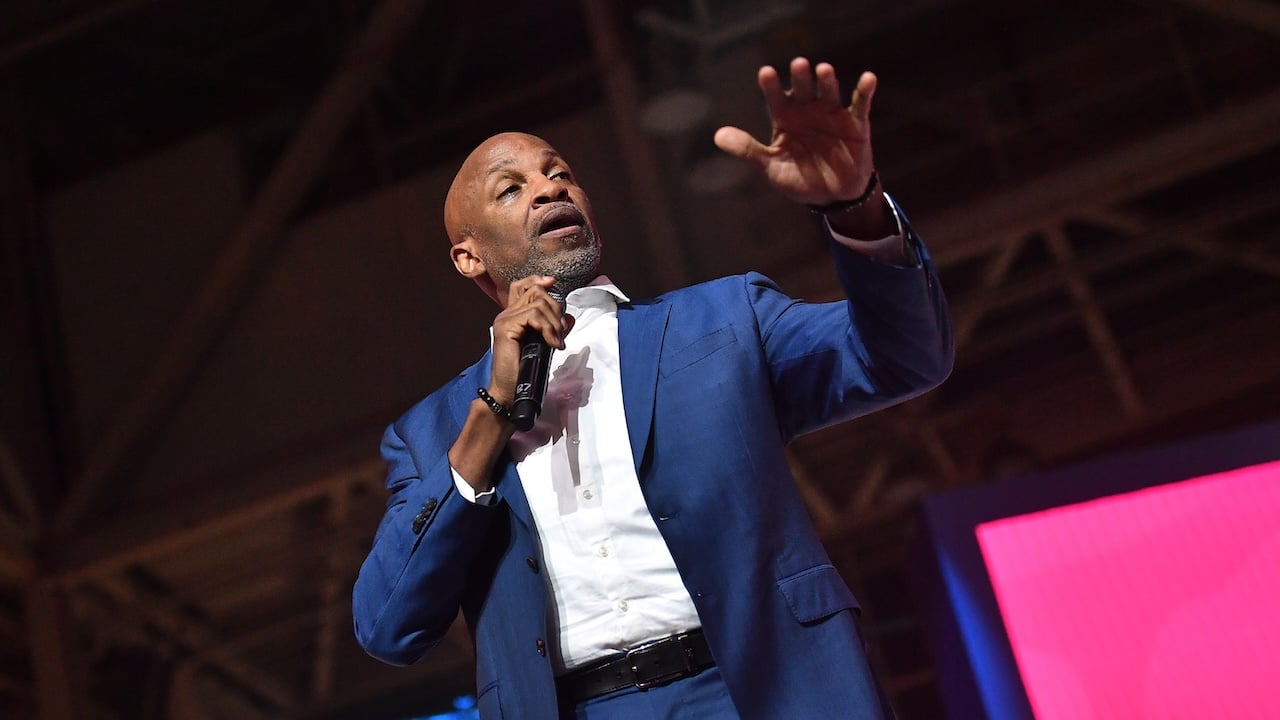
If you’re a person of a certain age and navigating “the change,” you may have seen social media posts commenting about perimenopause and menopause, or ‘cougar puberty,’ as some creatives have tagged it. Women’s health experts, such as Dr. LaKeischa McMillan, aim to help women understand the complexities of the “change of life” and empower them to receive the care they deserve.
Hailed as the International Menopause Whisperer, McMillan will join the National Menopause Show on Oct. 4-5 in Anaheim, Calif. She encouraged those in the area to attend because sometimes we need to give Dr. Google a rest.
“There are times when we can go down rabbit holes,” McMillan said. “[The National Menopause Show] is where you have an opportunity to listen to experts, innovators, and advocates to be able to get some real information that’s backed by science and not fear-mongering.”
As she experienced her own changes, McMillan was inspired to find new ways of sharing information, resources, and validation with women navigating the journey of perimenopause and menopause.
“I was able to take a step back, look at the way that my body’s changing, take that information and then show up to women’s health in a new and different way,” she said. “Now I can validate perimenopausal and menopausal women’s symptoms, help them crack their unique hormone code, and then provide a personalized symptom solution blueprint for them.”
But at the most basic level, McMillan said that, similar to the talk many people receive when they start puberty, there needs to be a talk 2.0 that helps women understand the changes they experience later in their reproductive life.
“The other PMS talk is the term I’ve actually coined where we talk about perimenopause, menopause syndrome, or system,” she shared. “Your body is going to change again. And I don’t think that we take the time to help women understand that piece.”
She said the second part of the process is having the “tough conversation” with your provider to see if they even understand or know about perimenopause and menopause. Research shows that most doctors receive little to no training about menopause, even in ob-gyn residency programs. A 2022 survey of 145 OB-GYN residency program directors found that fewer than one-third of the programs had a menopause curriculum in place.
According to McMillan, a space like the National Menopause Show can provide necessary information and guidance that’s evidence-based and on the cutting edge of medical innovations. She will lead a 101-style conversation that helps people begin to answer lingering questions or learn what questions to ask.
And one of the most central questions is how we even define and diagnose perimenopause and menopause.
“Menopause is 12 consecutive months without a period. That’s the definition,” she said. “Now, prior to that, there is something called perimenopause. And I call this purgatory because this is the time that can last 5, 7, 10, 15 years prior to menopause.”
She explained that the symptoms can impact your daily life, given the fluctuating hormones and other erratic changes.
“For instance, when progesterone starts dropping, your sleep can get interrupted,” McMillan said. “Or if your testosterone is dropping–and yes, women make testosterone, it is important for us–and now you’re starting to have brain fog because testosterone helps with brain health.”
Weight gain, loss of muscle mass, and insulin resistance are all symptoms of the hormonal shifts as your estrogen and testosterone levels fluctuate. Part of the importance of speaking with a provider who understands menopause and perimenopause is getting access to treatment and resources to manage symptoms.
McMillan approaches menopause care as a spectrum rather than having a specific endpoint. And contrary to popular belief, she shared that there is no one specific test that will determine if someone is or isn’t in perimenopause.
“There are various different ways to test different hormones in your body, mainly the ones that we look at are the ones that are considered your sex hormones,” she explained. “Then there are some other tests that practitioners may even layer on, which I call functional medicine type of testing, where you get all of that data.”
As a practitioner, McMillan adopts an integrative approach, which provides a more comprehensive picture. She said that evaluating the person’s symptoms, along with various hormones such as estrogen, progesterone, testosterone, and follicle-stimulating hormone, can provide a more comprehensive picture of what is going on.
When asked about the use of hormonal replacement therapies, McMillan discussed the evolving understanding of contemporary treatment options. For years, medical professionals told women that hormone replacement therapy could increase their risk of breast cancer and other health issues. But recent re-evaluations of a 2002 study and updated analysis suggest that today’s hormonal therapy, relying primarily on “biodentical” and not synthetic sources, offers many benefits to women navigating perimenopause and beyond.
“We have done a disservice to two generations of women for over 20 years,” she said. “We know that these hormones have cardiovascular protection, they have brain protection, they have breast protection. They have bone protection and colorectal protection.”
From a practical standpoint, she has stopped using the word postmenopausal because it doesn’t have a standard definition, the same as menopause. While many use the term to indicate the end of something, McMillan said it hides the fact that women will continue to experience changes even after “the change.”
“You are going to spend the last third of your life in this menopausal phase of life,” she explained. “And you have to now figure out what tools I need to help every time my body changes because there’s going to be a change in relationship to my physiology.”
She noted that for women who experience postmenopausal bleeding, it is necessary to rule out endometrial cancer or other conditions.
“Now, postmenopausal bleeding does not automatically mean endometrial cancer,” she emphasized. “It’s just the big ugly thing that [needs to be] ruled out.”
McMillan emphasized asking the right questions and reflecting on your current provider’s approach to determine whether you need additional or different care. She stressed the importance of advocating for yourself and feeling comfortable enough to share any concerns or issues that need attention.
“Walk into the doctor’s office and say, I know I’m different. I know there’s a change, and how do we take care of this?” she said. “Then, understanding that this is a very complex time in your life. This is very layered, and it’s going to look different for everybody. That’s the key. There’s no one-size-fits-all.”
Tickets are on sale now at nationalmenopauseshow.com. Use the code MENOPAUSE20 for 20 % off. A one-day pass costs $45, and a two-day pass costs $55.
SEE ALSO:
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0